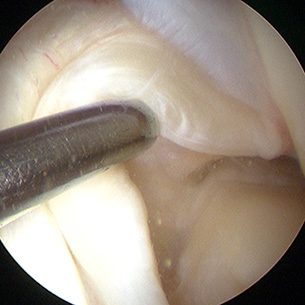
Left Knee arthroscopy - Stretched out and incompetent ACL being tested at the time of arthroscopy.
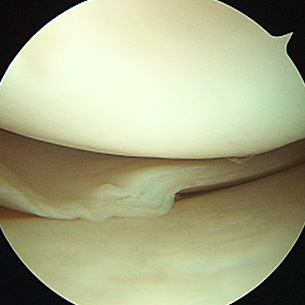
A torn medial meniscus (inner cartilage).
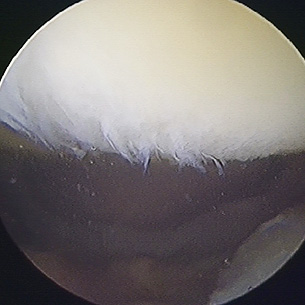
Early osteoarthritis of the back of the kneecap (patella).
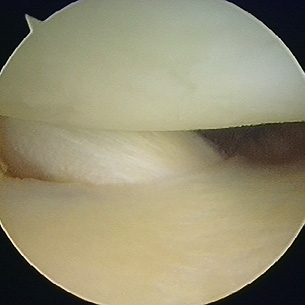
Small tendon at the back of the knee, the popliteus tendon, frequently seen at knee arthroscopy. It can occasionally tear.
The arthroscope has revolutionised modern orthopaedic surgery. Frequently referred to as `keyhole surgery' it is now a skill that most orthopaedic surgeons have acquired by the end of their training. However, the use of keyhole surgery is not new. As long ago as 1806, a device known as the lichtleiter was used to inspect the rectum and vagina. The lichtleiter had two canals, one for the light, normally a candle, and the other a viewing tube. Throughout the 19th century all manner of devices appeared for looking into various parts of the human anatomy. In 1918 a viewing tube normally reserved for inspecting bladders was inserted into a knee joint by a Japanese surgeon - the arthroscope had been born. The profession was fairly sceptical at the time. Look at the statement put forward by a Dutch surgeon in 1937:
"How can anyone venture to introduce a luminous object into a knee joint in an effort to look between the articular surfaces, which cannot be separated. This is quite impossible. Moreover, this procedure is more dangerous than exploratory arthrotomy."
How times have changed! Knee arthroscopy is now one of the commonest, if not the commonest orthopaedic operation performed in the developed world today.
The Equipment
An arthroscope is basically a cylinder with a lens at each end. Because this viewing tube is so delicate the device is sheathed by a cannula for protection. Using a fibreoptic viewing system it is possible for light to be shone down the arthroscope in the same direction as the surgeon is viewing in order to illuminate the interior of the joint. Most arthroscopes used in knee surgery do not actually view directly ahead, but at an angle of 30 degrees from the line of the arthroscope.
This allows a surgeon to look around corners - there are plenty of them in a knee. A camera is usually attached to the viewing end of the arthroscope and the image displayed on an adjacent television screen. Instruments can then be introduced into the knee through separate holes (surgical holes are sometimes called 'portals') so that tissue can be removed or repaired. These instruments can be manually operated, or powered, radiofrequency, or even lasers.
Indications for Surgery
At its simplest, an arthroscope can be used for diagnosis. However, now it is more usual for it to form part of sometimes quite complex operations. Some of these are as follows:
- Torn cartilage (meniscus)
- Fractures
- Ligament injuries (e.g. anterior and posterior cruciate ligaments)
- Retrieving loose bodies
- Synovectomy
- Arthritis (osteoarthritis and rheumatoid arthritis)
- Debridement (surgical cleaning)
- Anterior knee pain
- Knee infection
- Bursitis
- Problematic knee replacement
- Etc., etc. etc…
The advantage of the arthroscope is its low complication rate and short hospitalisation time. The disadvantage is that arthroscopy is technically demanding, requires expensive equipment, and sometimes access to certain parts of the knee is difficult. Nevertheless, knee arthroscopy is a welcome addition to the orthopaedic repertoire. Without it many significant advances in knee surgery would not have occurred.
